Should you see a chiropractor if you are pregnant?
Easy answer. YES! As any woman who has had a child can tell you, your back hurts when you are pregnant. Pregnancy is a very stressful time for the body, especially the low back, mid back, and pelvis. First of all, you gain a good deal of anterior weight. There is another person in there. That alone is enough to throw things out of whack.
As the abdomen expands and gets heavier, the lumbar spine begins to curve more than normal causing the muscles around the spine to become tighter in an attempt to balance out the stresses. Visiting a chiropractor can help address these issues and teach you how to cope with your new, temporary body.
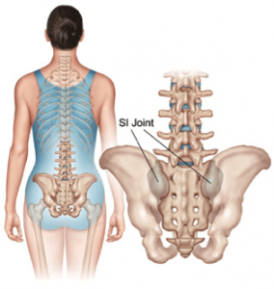
Probably the most common spine-related problem with pregnancy is lack of motion of the pelvis. The joint that connects your pelvis to your tailbone (the sacroiliac or “SI” joint) tends to lose some of its normal motion with pregnancy as the pelvis starts to expand to adapt to the growing fetus. These joints are crucial for proper pelvic mobility before, during, and after delivery. Regular chiropractic adjustments during pregnancy can help keep joints mobile and prevent a lot of issues such as pain, intrauterine constraint, and abnormal fetal positioning.
Further, there are muscles that act on the the hip and pelvis that can get extremely tight and cause shooting nerve pain, numbness, and/or tingling down the leg during pregnancy. By working to stretch these muscles and doing at-home exercises, these symptoms can be managed or even prevented.
Is chiropractic care during pregnancy safe?
Absolutely! Obviously we aren’t going to just lay you on your stomach and jump on you as hard as we can when you are about to pop. There are a variety of ways a chiropractor can treat pregnant women that is safe for both the mother and the baby.
With the trending shift towards alternative medicine and more natural treatment choices, many healthcare providers are finding local chiropractors to refer their pregnant patients to. If you are pregnant or plan on becoming pregnant seek out a chiropractor or consult your other healthcare providers about the benefits of chiropractic.